Some insurers, including government-run Medicare, refused to pay for the drug until it received full approval.
U.S. authorities on Thursday granted full approval to a closely watched Alzheimer’s disease drug, paving the way for government-run Medicare and other insurance plans to begin covering the treatment of people with brain stealing disease.
The Food and Drug Administration (FDA) has approved the IV drug Leqembi for patients with mild dementia and other symptoms caused by early-onset Alzheimer’s disease. It is the first drug that has been convincingly shown to slightly slow the cognitive decline caused by Alzheimer’s disease.
Japanese drugmaker Eisai received conditional FDA approval in January based on early results suggesting Leqembi worked by removing sticky brain plaque linked to the disease.
The FDA confirmed these findings by examining data from a larger study of 1,800 patients in which the drug slowed memory and thinking decline by about five months in those who received the treatment, compared to those who received a placebo.
“This confirmatory study has confirmed that it is a safe and effective treatment for patients with Alzheimer’s disease,” FDA Neurological Drugs Director Dr. Teresa Buracchio said in a statement. communicated.
The medicine’s prescribing information will contain the most serious type of warning, stating that Leqembi can cause brain swelling and bleeding, side effects that can be dangerous in rare cases. The label notes that these issues are also seen with other plaque-targeting Alzheimer’s drugs.
The process of converting a drug into full FDA approval typically gets little attention. But Alzheimer’s patients and advocates have been lobbying the US federal government for months after Medicare officials announced last year that they would not pay for the routine use of drugs like Leqembi until that they would not have received full FDA approval.
It was feared that the cost of new Alzheimer’s drugs targeting plaque could overwhelm the finances of the programme, which provides care for 60 million elderly people. Leqembi costs about $26,500 for a year’s supply of IVs, which are given every two weeks.
The vast majority of US citizens with Alzheimer’s disease obtain health coverage through Medicare. And private insurers have followed suit by withholding coverage for Leqembi and a similar drug, Aduhelm, until they receive full FDA approval.
An FDA decision on full approval of Aduhelm is still years away.
Medicare Administrator Chiquita Brooks-LaSure said in a statement Thursday that the program will begin paying for the drug now that it has full FDA approval. But the government also sets additional requirements, including listing on a federal registry to track the drug’s actual safety and effectiveness.
Medicare “will broadly cover this drug while continuing to collect data that will help us understand how the drug works,” Brooks-LaSure said.
Some Medicare patients might be required to pay the standard 20% of Leqembi’s cost, though the amount varies depending on their plans and other coverage details.
Hospitals and medical clinics have warned that it could take time for people to start taking the drug.
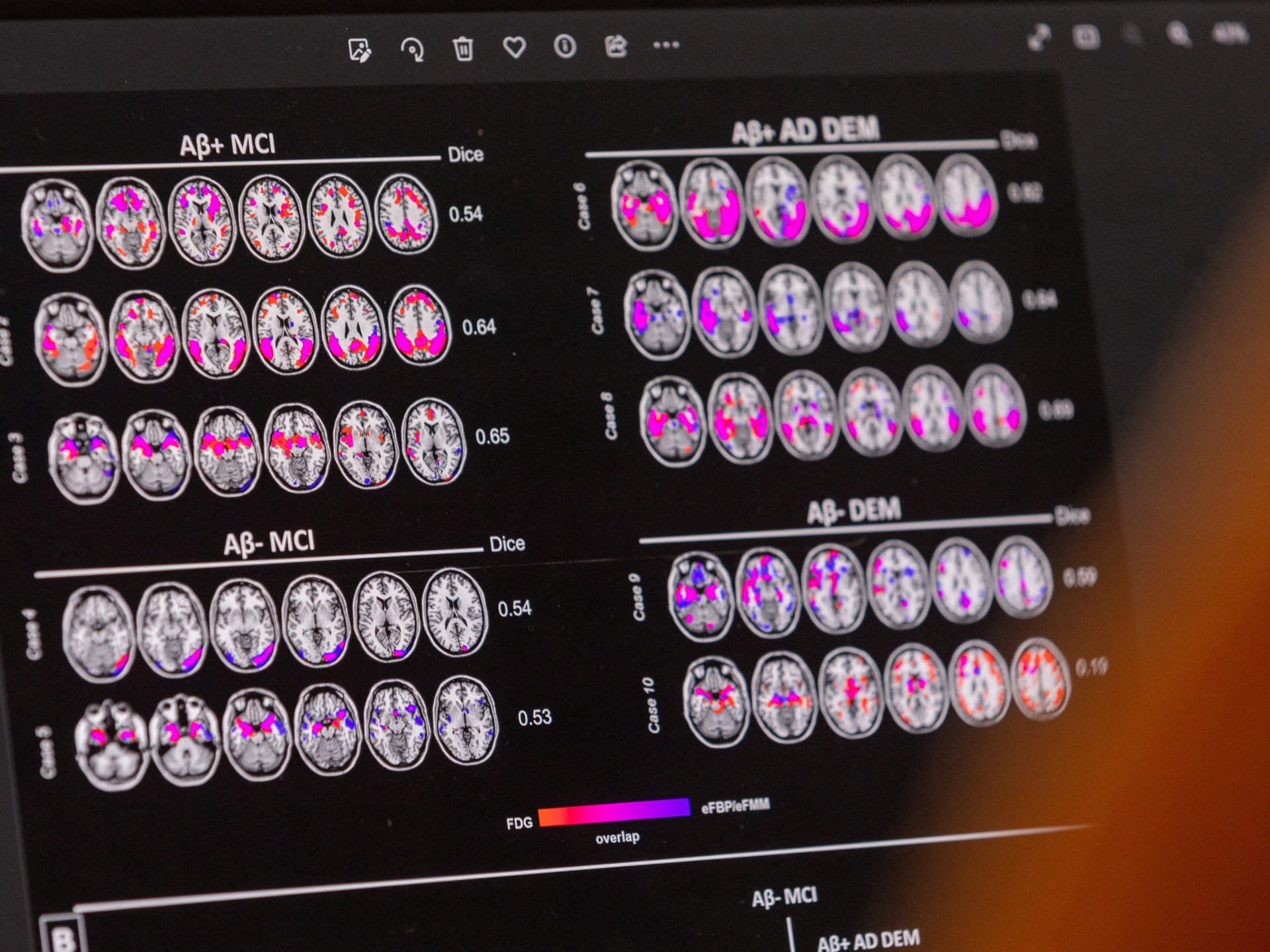
Physicians should confirm that patients have the brain plaque targeted by Leqembi before prescribing it. Nurses should be trained to administer the drug, and patients should be monitored with repeat brain scans to check for swelling or bleeding. Imaging and administration services result in additional costs to hospitals beyond the drug itself.
Eisai told investors that approximately 100,000 Americans could be diagnosed and eligible to receive Leqembi by 2026. The drug is co-marketed with Biogen, a Cambridge, Massachusetts-based company.
“We want to make sure that only the right patients receive this product,” said Alexander Scott, Vice President of Eisai.
Eisai studied the drug in people with early or mild disease who were assessed using a scale measuring memory, thinking and other basic skills. After 18 months, those who received Leqembi declined more slowly – a difference of less than half a point on the scale – than participants who received a sham infusion.
Some Alzheimer’s experts say the delay is probably too subtle for patients or their families to notice. But federal health advisers said the difference could still be significant and recommended that the FDA fully approve the drug at a public meeting in June.